A 32 yr old male with vomiting and fever since 2 days
V Sai Jaya Krishna,Intern
Roll no 158
"This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
32 yr old male with vomiting and fever since 2 days
A 32 yr old male came to OPD with
Chief complaints of :
- vomiting since 2 days
- generalised weakness since 2 days
- 1 episode of fever low grade since yesterday night
- chest pain(diffuse) since yesterday
HISTORY OF PRESENT ILLNESS :
- Patient was apparently asymptomatic 2days back , he had 20 episodes of vomiting which were non projectile,non bilious and 10 episodes were and then he had developed diffuse chest pain and abdominal pain since 2 days.patient had c/o fever which has releived on taking medication.
PAST HISTORY :
- Not a k /c/ o Dm,HTN , Thyroid , TB , Asthma Epilepsy , CVA .
Family history : not significant .
PERSONAL HISTORY :
Diet - mixed
Appetite - reduced since 4 days
Bowel movements - regular, bladder - regular
Sleep - adequate
Addictions : consumes alcohol occasionally since 5yrs.
- No smoking
- No allergies
GENERAL EXAMINATION :
- Patient was examined after taking his consent
- Patient is conscious , coherent , cooperative , well oriented to time , place and person .He is moderately built and nourished
- No signs of pallor , icterus , cyanosis , clubbing , oedema , lymphadenopathy .
His vitals:
Temperature : 99.2F
BP : 120/80 mm HG
Pulse rate : 70bpm
Resp.rate : 26cpm
GRBS : 118mg/dl
Spo2 : 98 percent
Systemic Examination:
CVS- S1 S2 heard,no murmurs present.
RS - bilateral Air entry present
Normal vesicular breath sounds heard
Per Abdomen : soft , tenderness +Rt iliac fossa,Rt hypochondrium ,Lf hypochondrium , bowel sounds - , no signs of organomegaly
CNS :higher mental functions : normal
Reflexes :
MOTOR-: normal tone and power
reflexes:
RT L T
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
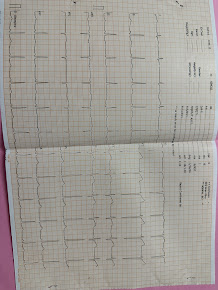
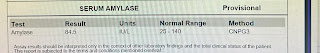
Investigations:
ECG
Hemogram
CUE
Electrolytes
LFTSerum amylase
Provisional diagnosis :
Alcohol gastritis
Treatment :
1 inj pan 40 mg IV/OD
2 Inj zofer IV/TID
3. Inj . thiamine 200 mg in 100 ml NS IV/ BD
4.Iv fluids NS
RL @100 ml /he
5)Inj pan 80 mg in 100 ml NS /IV/stat given