55YR OLD PATIENT WITH CKD ON MHD
"This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
Chief complaints-
Complaints of shortness of breath since 2 months and pain in lower back since 2 months.
HOPI-
Patient was apparently asymptomatic 2 months back then he had sudden onset of shortness of breath which was insidious in onset grade 2 gradually progressed to grade 4 aggrevated on doing work.ORTHOPNEA and PND present.
No fever ,chest pain.
Decreased urine output since 2 months.Thin stream.poor flow,increased frequency,hesitancy,burning micturition present.
Past History-
K/C/O DM since 20 yrs.
K/c/o HTN since 6 months.
Not a k/c/o TB,Epilepsy,CVA, CAD, Bronchial Asthma, Thyroid Disorders.
Personal History:
Diet- Mixed
Appetite- normal
Bowel & Bladder Movements- regular
Sleep - Adequate
Addictions - None
Family History -
Not significant
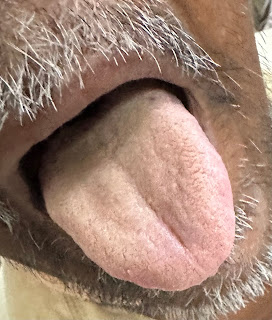
General Examination: