64 yr old male with lower respiratory tract infection
"This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
A 68YR OLD MALE CAME TO OPD WITH CHIEF COMPLAINTS OF COUGH AND HEADACHE since 1 week
History of present illness::
Patient was apparently asymptomatic 1 week ago then he developed COUGH initially dry later progressively expectoration started white in colour moderate quantity ,non foul smelling,not blood stained, no nocturnal and diurnal variation , relieved on medication with SOB grade 3 with fever since 4 days low grade ,sore throat present.
H/o polyuria and polydypsia since 1 week.
No H/o wheez, chest pain, palpitations.
H/o loss of appetite since 1 day.
Headache in parietal region,full aching type not with photophobia,phonophobia.
No h/o vomiting,abdominal pain,constipation,loose stool,giddiness ,blurring of vision.
PAST HISTORY :
-k /c/ o HTN since 5 yrs and on amlong 10.
-No h/o DM,Thyroid , TB , Asthma Epilepsy , CVA .
Family history : not significant .
PERSONAL HISTORY :
Diet - mixed
Appetite - reduced since 1day
Bowel movements - regular, bladder - regular
Sleep - adequate
Addictions : consumes alcohol occasionally since 10 yrsyy.
- No smoking
- No allergies
GENERAL EXAMINATION :
- Patient was examined after taking his consent
- Patient is conscious , coherent , cooperative , well oriented to time , place and person .He is moderately built and nourished
- No signs of pallor , icterus , cyanosis , clubbing , oedema , lymphadenopathy .
RFT:
Vitals..
Pulse:80bpm
Bp:140/80 mm of hg
Temperature::afebrile
RR:16c/min
Systemic examination
Respiratory examination
Inspection-
B/L symmetrical and elliptical
Trachea appears to be central
No supraclavicular and infraclavicular hallowing present
Expansion of chest equal on both sides
Expansion of chest normal
No crowding of ribs
No drooping of shoulder
No Wasting of muscles present
No scoliosis ,kyphosis
No sinuses,scars,engorged veins
Palpation-
No local rise of temperature
All inspectory findings confirmed
Trachea central
Apex beat felt in 5th ICS in mid clavicular line
Percussion-
Direct : over clavicle and manubrium sternum
Indirect :
Right. Left.
Supraclavicular. Resonant. Resonant
Infraclavicular. Resonant. Resonanat
Mammary. Resonant. Resonant
Inframammary. Resonant. Resonanat
Axillary Resonant. Resonant
Infraaxillary. Resonant Resonant
Suprascapular. Resonant. Resonant
Interscapular. Resonant Resonant
Infrascapular. Resonant. Resonant
Auscultation-
B/L air entry present
Normal vesicular breath sounds heard
CVS-
S1 S2 heard,no murmurs present.
Per Abdomen :
soft , Non tender , bowel sounds + ,
no signs of organomegaly
CNS :
higher mental functions : normal
MOTOR-: normal tone and power
reflexes:
RT L T
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
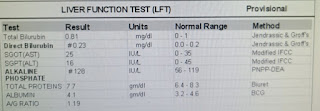
Investigations:
Provisional diagnosis:
Lower respiratory tract infection?